Pinched Nerve: What To Do For Sciatica and Lower Back Pain

Are you wondering how doctors determine the location of a pinched nerve? Which tests are the most effective for pinpointing the problematic nerve? And what can you do to alleviate the discomfort caused by a trapped nerve?
It’s not uncommon to receive numerous emails daily from individuals sharing their MRI reports, often lacking information about their medical history or examination. In this article, we’ll explore the methods doctors use to diagnose pinched nerves and offer guidance on managing this condition.
Navigating Sciatica Queries
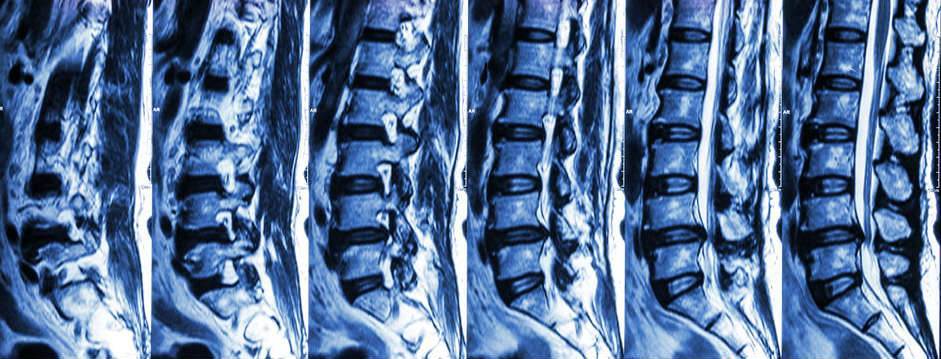
Individuals facing the challenge of sciatica often seek guidance on the most suitable course of action. Questions about surgery or exercises to “cure” the problem are common. However, providing advice based solely on an MRI is challenging, as an MRI alone does not constitute a definitive diagnosis and can often be inaccurate.
The MRI Dilemma
Despite being considered a gold standard in some contexts, research has revealed a lack of correlation between MRIs and pain. While MRIs are highly sensitive, their specificity is limited. In simpler terms, an MRI may reveal various abnormalities, yet these findings may not necessarily be linked to the pain. It’s not uncommon to observe multiple disc herniations on an MRI, with only one or none of them contributing to the pain.
“It is very rare for an MRI. to come back with the words ‘normal study,“ said Dr. Christopher DiGiovanni, a professor of orthopaedics and a sports medicine specialist at Brown University. “I can’t tell you the last time I’ve seen it.” From the New York Times
Where Is My Pinched Nerve?

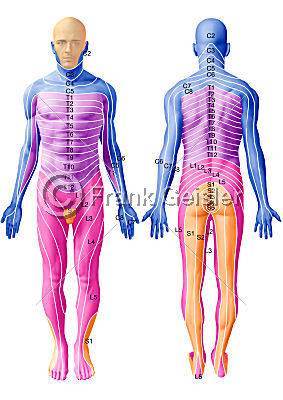
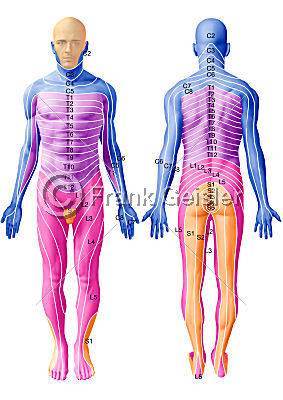
Dermatomes Help Determine Where Your Pinched Nerve Is
Skin sensations like tingling, numbness and pain called dermatomes help pinpoint where your pinched nerve is. These specific skin areas correspond to individual spinal nerves, such as the S1 nerve covering your little toe, other toes, and Achilles area, as well as the L5 nerve serving your big toe, the top of your foot, and the side of your lower leg. Each nerve has its designated dermatome.
Understanding Dermatomes: Consistency and Variations
Dermatomes, the specific areas of skin innervated by spinal nerves, offer reliable diagnostic insights. However, like the uniqueness of individual noses, dermatomes may exhibit slight variations among people. These variations, though present, do not diminish the overall consistency of dermatome patterns, making them a valuable tool in diagnostic assessments.
Enhancing Diagnostic Precision: Dermatomes vs. Neurological Examination
In cases of sciatica, a thorough neurological examination traditionally assesses reflexes, muscle strength, and skin sensitivity.[1-2] Dermatomes, on the other hand, provide an additional layer of diagnostic precision. Research suggests that dermatomes align with textbook descriptions in a significant majority of cases, making them a dependable resource for healthcare professionals.
The Reliability Factor: Dermatome Consistency and Uncommon Variations
Studies indicate that dermatomes correspond to textbook descriptions approximately 88% of the time for the L4 nerve, 82% for the L5 nerve, and 83% for other nerves. While these percentages demonstrate a strong correlation, it’s essential to acknowledge that a small percentage of individuals may exhibit dermatomes in unexpected locations. Despite these rare variations, chiropractors rely on their expertise and a comprehensive evaluation of multiple diagnostic factors to ensure accurate diagnoses. Ultimately, the occasional divergence in dermatome positioning does not significantly impact the diagnostic process’s overall reliability.
L4 Dermatome
Impact on L4 Dermatome: Diagnoses and Conditions
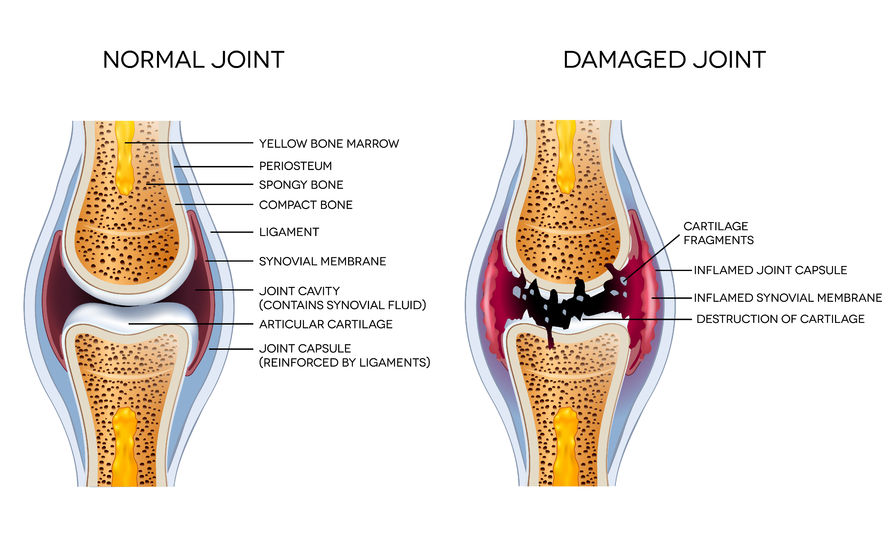
The L4 dermatome can be influenced by various diagnoses, including disc herniations, osteoarthritis, and degenerative disc disease. Additionally, conditions like lateral stenosis, often caused by spinal joint bone spurs, can contribute to issues related to the L4 dermatome.
Understanding the L4 Disc: L4 Pinched Nerve
Situated between the L3 and L4 vertebrae, the L4 disc houses the L4 nerve, which runs between them. Compression of the L4 nerve typically results in pain radiating to the big toe and the inner part of the shin, just above the ankle. This discomfort may extend along the front of the shin and even reach the side of the thigh.
Assessing Nerve Compression: Weakness in Quadriceps Muscles
Nerve compression in the L4 dermatome can lead to weakness in the quadriceps muscles, affecting the nerve segment responsible for muscle control. This weakness can impact daily activities such as squatting, posing challenges due to compromised nerve function.
L5 Dermatome
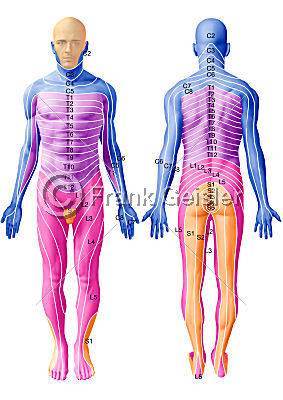
L4-L5 Disc and L5 Nerve: Understanding the Anatomy
Located between the L4 and L5 vertebrae is the L4-L5 disc, with the L5 nerve emerging between these adjacent vertebrae.
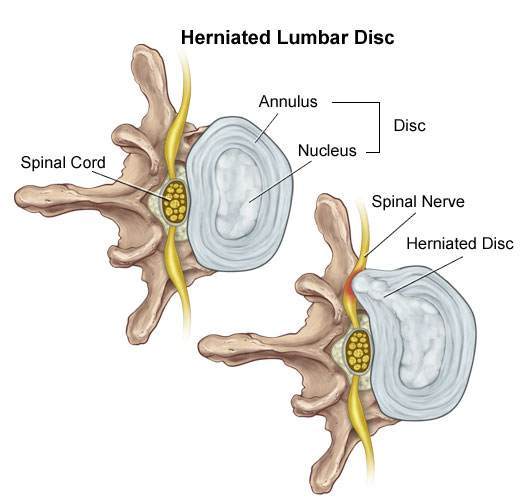
Disc Herniation Patterns: Forward and Backward
Discs in your spine can herniate in various directions, including forward, backwards, and sideways. Typically oval when viewed from above, discs can herniate within a 360-degree circle. Fortunately, disc herniations tend to follow a common pattern, often protruding backwards and slightly away from the centre. This specific type of herniation is known as paramedian (or paracentral) or lateral recess herniation.
Side Disc Herniation: Common Occurrence
One common way for discs to herniate is through the side portion of the disc, which is often the weaker point due to the presence of the posterior longitudinal ligament (PLL) located directly behind the disc. The PLL, situated posteriorly, provides structural support.
Influences on Herniation Direction: Anatomy and Activities
The direction of disc herniation is influenced by both spinal anatomy and daily activities. Frequent forward bending, such as when shaving, applying makeup, or lifting objects, exerts pressure on the front of the disc. This pressure can cause the jelly-like substance inside the disc to protrude towards the back. Given the central location of the PLL, herniations often occur slightly to the right or left going off to the side.
Paramedian and Lateral Recess Herniations
The terms “paramedian” and “lateral recess” both describe disc herniations that occur near the midline but are slightly off-centre. In paramedian or paracentral herniations, the disc protrudes close to the midline on either side of the centre, while lateral recess herniations involve the disc pushing out to the side toward the nerve as seen below.
Symptoms of L4-L5 Disc Herniation
When an L4-L5 disc herniates in a paramedian, paracentral, or lateral recess fashion, approximately 82% of individuals may experience pinched nerve effects. This often includes sensations originating from the big toe, extending along the top of the foot, the outer shin, up the side of the thigh, and reaching the buttock and the L5 vertebrae area.
Muscle Damage and Foot Drop
Damage to the muscle portion of the L5 nerve can result in foot drop, a condition where the toes consistently strike the floor, making it challenging to lift them. This altered walking pattern may lead to the affected foot being lifted higher to compensate, potentially increasing the risk of tripping and falling.
S1 Dermatome
L5-S1 Disc Herniation Patterns
The L5-S1 disc commonly herniates in the paramedian, paracentral, or lateral recess region. It’s important to note that paramedian and paracentral both refer to a disc herniating next to the centerline.
Effects of L5 Nerve Compression
In approximately 83% of cases involving disc herniation in the paramedian or lateral recess area, the L5 nerve becomes compressed. This compression often leads to sensations of burning, numbness, or pain starting from the baby toe and extending towards the heel, up the side or back of the leg, and further along the thigh to the buttock.
Muscle Control and Reflex
When the part of the nerve responsible for muscle control is affected by compression, you may encounter difficulties performing activities like doing ten or more heel raises. Additionally, the Achilles reflex, which involves the contraction of calf muscles upon tapping the Achilles tendon, may be absent.
Empowering Knowledge
Providing you with this information aims to empower you, enabling a better understanding of the general aspects of your pinched nerve, whether it’s associated with disc herniations, stenosis, or degenerative changes due to osteoarthritis.
Feel free to share your questions, thoughts and experiences in the comments below, and don’t forget to connect with us on Facebook for more updates and tips on improving your shoulder health. We’d love to hear your opinions on who you consider the best Toronto chiropractor.
Research
1. Quraishi NA,Taherzadeh O,McGregor AH, Hughes SP, Anand P, Correlation of nerve root pain with dermatomal sensory threshold and back pain with spinal movement in single level lumbar spondylosis. J Bone Joint Surg Br. 2004 Jan;86(1):74-80.
2. Hancock MJ, Koes B, Ostelo R, Peul W. Diagnostic accuracy of the clinical examination in identifying the level of herniation in patients with sciatica. Spine 2011; 36:E712-E719.
3. Nitta H, et al. “Study on dermatomes by means of selective lumbar spinal nerve root block.” Spine 1993;18:1782-1786.