Patellofemoral Pain Syndrome (PFPS): Causes and Considerations for Triathletes in Toronto

Patellofemoral Pain Syndrome (PFPS): Causes, Symptoms, Prevention, and Treatment
Patellofemoral Pain Syndrome (PFPS), commonly known as “runner’s knee,” is prevalent among triathletes and is characterized by pain around or behind the kneecap. This discomfort often intensifies during running, squatting, climbing stairs, or prolonged sitting. For triathletes in Toronto, consulting a chiropractor can be instrumental in diagnosing and managing PFPS effectively.
Detailed Causes of Patellofemoral Pain Syndrome in Triathletes
Overuse and Repetitive Stress
Overuse and Repetitive Stress: High-impact activities such as running, cycling, and swimming can subject the knee joint to repetitive stress, leading to irritation under the kneecap. As noted by the Mayo Clinic, this overuse is a primary contributor to patellofemoral pain syndrome (PFPS). Repetitive motion and impact can strain the knee structures, causing pain and discomfort over time.
Muscle Imbalances or Weaknesses
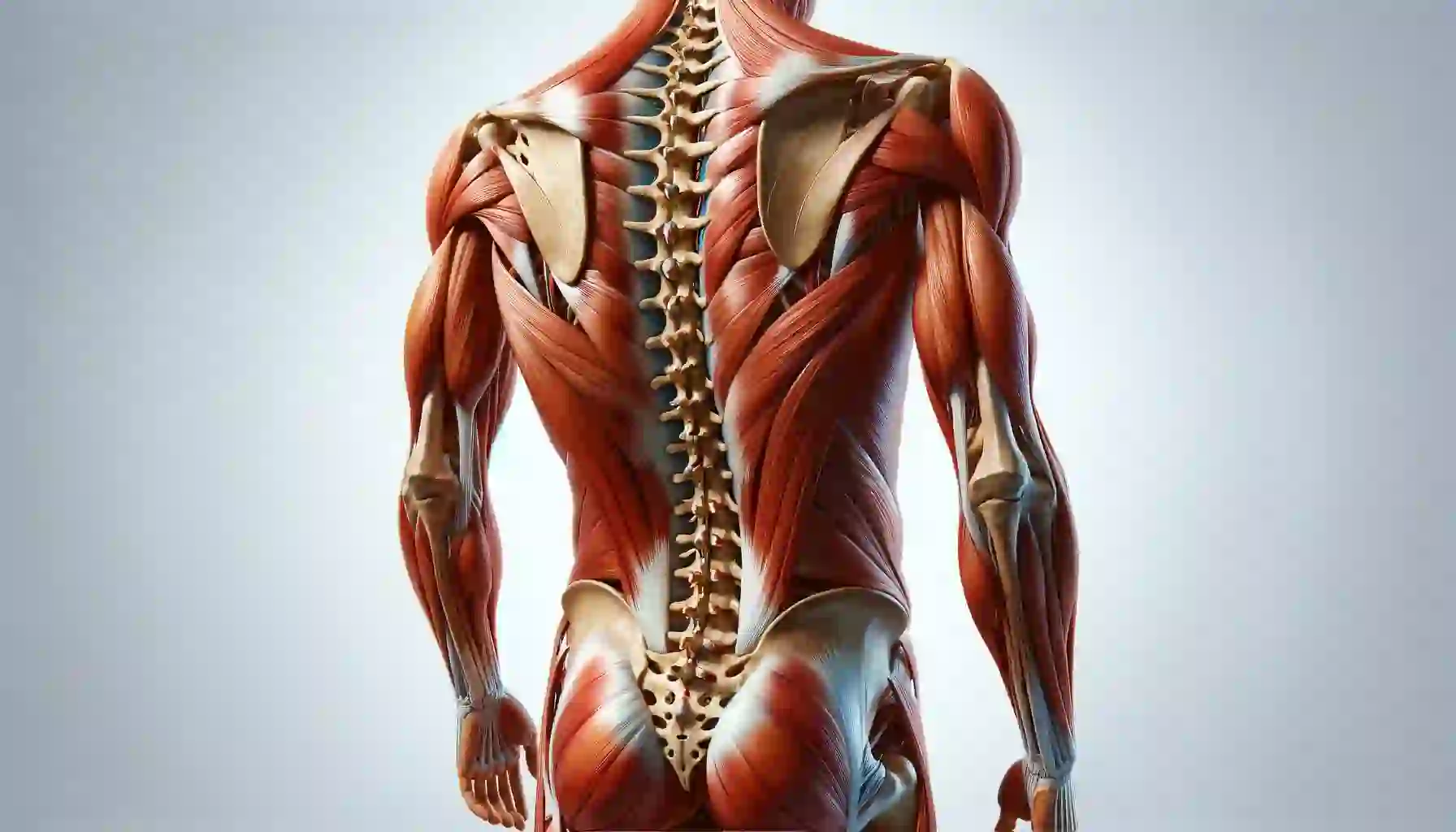
Muscle Imbalances or Weaknesses: Weakness or tightness in the quadriceps muscles, especially the vastus medialis obliquus (VMO), can disrupt proper kneecap tracking, increasing the risk of PFPS. Similarly, weak hip abductors and external rotators can alter biomechanics, placing additional stress on the knee joint. This imbalance can cause improper alignment and movement patterns, exacerbating knee pain.
Improper Training Techniques
Improper Training Techniques: Sudden training intensity or duration increases without adequate preparation can strain the knee joint. Rapid escalation in physical activity can overwhelm the knee’s ability to adapt, leading to PFPS. Additionally, poor running form, such as excessive foot pronation or supination, can contribute to the development of PFPS by causing uneven stress distribution across the knee joint.
Structural Abnormalities
Structural Abnormalities: Flat feet, or pes planus, can lead to improper knee alignment, increasing stress on the patellofemoral joint. This structural issue can result in the knee compensating for the lack of proper foot support, thus aggravating PFPS. Kneecap misalignment, such as patellar maltracking, can predispose individuals to PFPS by causing uneven wear and tear on the knee structures.
Inadequate Footwear
Wearing shoes that lack proper support or are inappropriate for specific activities can exacerbate knee stress, contributing to Patellofemoral Pain Syndrome (PFPS). Inadequate footwear may fail to provide necessary stability and cushioning, leading to increased strain on the knee joint during physical activities.
To mitigate the risk of PFPS, selecting footwear that offers adequate support and is suitable for your specific activities is essential. This includes ensuring proper arch support, cushioning, and stability to reduce undue stress on the knee joint.
Previous Injuries
Previous Injuries: Past knee injuries can alter joint mechanics, increasing the risk of developing PFPS. Injuries can lead to compensatory movement patterns and weakened muscles, which can strain the knee and contribute to persistent pain and dysfunction. Individuals with a history of knee injuries need to follow proper rehabilitation protocols to avoid the recurrence of PFPS.
Specific Considerations for Triathletes
- Cycling: Prolonged cycling, especially in an aggressive riding position, can lead to knee pain if the bike is not properly fitted or if the rider has weak hip flexors or quadriceps.
- Swimming: While swimming is generally low-impact, repetitive kicking can strain the knee joint, especially if the swimmer has poor technique or weak hip flexors.
Recognizing and Preventing Patellofemoral Pain Syndrome (PFPS) in Triathletes
Patellofemoral Pain Syndrome (PFPS), commonly known as “runner’s knee,” is prevalent among triathletes and is characterized by pain around or behind the kneecap. This discomfort often intensifies during running, squatting, climbing stairs, or prolonged sitting. For triathletes in Toronto, consulting a chiropractor can be instrumental in diagnosing and managing PFPS effectively.
Symptoms of Patellofemoral Pain Syndrome
Recognizing the symptoms of PFPS is crucial for early intervention and effective management. Common symptoms include:
Anterior Knee Pain:
Aching or sharp pain localized around or behind the kneecap, particularly noticeable during activities that involve knee bending, such as running, squatting, or climbing stairs. This pain can hinder performance in running and cycling segments, where knee flexion is frequent.
Swelling:
Mild swelling or puffiness around the knee joint may be accompanied by tenderness to touch. Swelling can limit the range of motion and cause discomfort during training sessions.
Grinding or Clicking Sensation (Crepitus):
A sensation or audible sound of grinding, clicking, or popping when bending or straightening the knee. This can be distracting and indicate cartilage wear, affecting overall knee function.
Pain After Prolonged Sitting (Theater Sign):
Discomfort or stiffness in the knee worsens after sitting with bent knees for extended periods, such as during long meetings or flights. This symptom can affect recovery periods and daily activities, leading to prolonged discomfort.
Weakness or Sensation of Giving Way:
A feeling of knee instability or weakness, especially during weight-bearing activities. This can compromise performance and increase the risk of falls or further injury.
Prevention Strategies for Patellofemoral Pain Syndrome
Implementing preventive measures can significantly reduce the risk of developing PFPS. Key strategies include:
Rest and Recovery:
Allow adequate rest and recovery time between training sessions to enable tissue repair and adaptation.
Gradual Increase in Activity:
Slowly escalate the intensity and duration of physical activities to allow the body to adapt, reducing undue stress on the knee joint.
Proper Footwear:
Choose shoes that provide adequate support and cushioning and are appropriate for your activities.
Cross-Training:
Incorporate various exercises to prevent overuse of specific muscle groups and reduce repetitive knee stress.
Flexibility Training:
Engage in regular stretching routines to maintain muscle flexibility and joint range of motion.
Biomechanical Assessment:
Consult a sports medicine professional to assess your running or cycling biomechanics and identify potential issues.
Do It Yourself Treatment for Patellofemoral Pain Syndrome
Effective management of PFPS often includes:
Rest and Activity Modification
- Approach: Reduce or avoid activities that exacerbate pain to allow healing.
- Application for Triathletes: Temporarily decrease training intensity or switch to low-impact activities like swimming to minimize knee stress.
Exercise Therapy
Focus Areas: Engaging in targeted exercises to strengthen and balance the muscles around the knee.
Recommended Exercises:
Quadriceps Strengthening (Straight Leg Raises):
- How to Perform: Lie on your back with one leg bent and the other straight. Tighten the thigh muscle of the straight leg and lift it to the height of the opposite knee. Hold for a few seconds, then lower it slowly.
- Benefits: Strengthens the quadriceps without placing excessive stress on the knee joint.
Hip Abductor Strengthening (Side-Lying Leg Lifts):
- How to Perform: Lie on your side with the bottom leg bent for support. Keep the top leg straight and lift it upward without rotating the hip. Hold briefly, then lower it slowly.
- Benefits: Enhances hip stability and supports proper knee alignment.
Hamstring Stretch:
- How to Perform: Sit on the floor with one leg extended and the other bent. Reach toward the toes of the extended leg, keeping the back straight. Hold the stretch for 20–30 seconds.
- Benefits: Improves flexibility of the hamstrings, reducing tension on the knee.
Treatment From Health Professionals
Chiropractic Care
- Services Offered: In Toronto, chiropractors offer treatments such as manual therapy, myofascial release, and corrective exercises to address PFPS.
- Benefits: These therapies can improve joint mobility, reduce pain, and correct biomechanical imbalances contributing to PFPS.
Orthotic Devices
- Types: Using supportive devices like knee braces or custom orthotics to improve alignment and reduce stress on the knee.
- Application for Triathletes: Custom orthotics can correct foot mechanics, reducing knee strain during running and cycling.
Pain Management
- Methods:
- Cryotherapy: Applying ice packs to the affected area to reduce inflammation and numb pain.
- Medication: Taking nonsteroidal anti-inflammatory drugs (NSAIDs) as recommended to alleviate pain and inflammation.
- Considerations: Always consult with a healthcare professional before starting any medication regimen.
Education and Training Modification
- Purpose: Educating athletes on proper training techniques and body mechanics to prevent recurrence.
- Application for Triathletes: Incorporate cross-training, ensure proper warm-up and cool-down routines, and avoid sudden increases in training intensity.
Surgical Intervention
- Consideration: Reserved for severe cases where conservative treatments have failed.
- Procedures: May include realignment of the patella or removal of damaged cartilage.
- Recovery: Involves extensive rehabilitation and a gradual return to activity.
Strengthening Exercises for Patellofemoral Pain Syndrome (PFPS)
- Clamshells:
- Purpose: Strengthens the gluteus medius muscles, which help stabilize the hip and knee.
- How to Perform:
- Lie on your side with knees bent at a 90-degree angle and feet together.
- Keep your feet touching, and lift your top knee as high as possible without moving your pelvis.
- Hold for a second, then lower the knee back down.
- Repeat 10–15 times on each side for 2–3 sets.
- Wall Squats:
- Purpose: Engages and strengthens the quadriceps, hamstrings, and glutes.
- How to Perform:
- Stand with your back against a wall and feet about 6–12 inches away.
- Slowly slide down the wall until your knees are bent at approximately 45 degrees.
- Hold for 5–10 seconds, then return to standing.
- Repeat 15 times, several times a day.
- Reference: Cleveland Clinic Health.
- Hamstring Curls:
- Purpose: Strengthens the hamstrings, aiding in balanced muscle support around the knee.
- How to Perform:
- Stand upright and hold onto a stable surface for balance.
- Slowly bend one knee, bringing the heel toward the buttocks.
- Hold briefly, then lower the foot back down.
- Perform 8–12 repetitions on each leg.
- Calf Raises:
- Purpose: Strengthens the calf muscles, supporting proper foot mechanics and reducing knee strain.
- How to Perform:
- Stand with feet hip-width apart near a wall or stable surface for support.
- Slowly rise onto the balls of your feet, lifting your heels off the ground.
- Hold briefly, then lower back down.
Stretching Exercises for Patellofemoral Pain Syndrome (PFPS)
- Quadriceps Stretch:
- Purpose: Improves flexibility in the front thigh muscles, reducing tension on the knee.
- How to Perform:
- Stand upright and hold onto a stable surface for balance.
- Bend one knee and grasp the ankle, pulling the heel toward the buttock.
- Keep knees close together and back straight.
- Hold for 15–30 seconds; repeat 2–4 times on each leg.
- Hamstring Stretch:
- Purpose: Enhances flexibility in the back thigh muscles, aiding knee function.
- How to Perform:
- Lie on your back with one leg bent and the other straight.
- Lift the straight leg and hold the back of the thigh.
- Gently straighten the knee until a stretch is felt in the back of the thigh.
- Hold for 15–30 seconds; repeat 2–4 times on each leg.
- Calf Stretch:
- Purpose: Reduces tightness in the calf muscles, which can affect knee mechanics.
- How to Perform:
- Stand facing a wall with hands at eye level.
- Place one foot behind the other, keeping the back leg straight and heel on the floor.
- Bend the front knee and lean toward the wall until a stretch is felt in the calf of the back leg.
- Hold for 15–30 seconds; repeat 2–4 times on each leg.
Additional Tips for Recovery and Prevention
- Avoid Aggravating Activities: Avoid exercises like deep squats or lunges that place excessive stress on the knees during early rehabilitation stages.
- Consistency: Perform exercises regularly, ideally daily, for optimal results.
- Progress Gradually: Start with lower repetitions and sets, increasing as strength and flexibility improve.
Conclusion
If you experience persistent discomfort from Patellofemoral Pain Syndrome (PFPS) despite trying recommended exercises, consulting a knowledgeable Toronto chiropractor can provide targeted treatment to alleviate your symptoms. Proper care and management can help you return to your activities pain-free and improve your overall athletic performance.