What is Degenerative Disc Disease DDD? A Comprehensive Guide

Pain Clues: Could Degenerative Disc Disease (DDD) Be the Cause?
- Do you have leg pain or weakness that spreads from your back?
- Is bending forward painful, while bending backwards brings relief?
If you answered yes, Degenerative Disc Disease or DDD might be behind your discomfort. This issue of Bodi Empowerment delves into DDD: causes, why pain happens, imaging interpretations, and treatment choices.
Treatments for Degenerative Disc Disease
Options range from conservative care (chiropractic, exercise) to surgical interventions like discectomy, fusion, or disc replacement.
Beware: X-rays Don’t Tell the Whole Story
Yes, your doctor found evidence of degenerative disc disease (DDD) on your X-rays or MRI. But here’s the surprise: research shows the severity of DDD visualized on images doesn’t directly tie to your pain level!
- Careful Diagnosis Matters: Doctors must go beyond imaging, using your health history and exam to pinpoint the true pain source.
- Pain Varies Wildly: A person with significant DDD on scans might have mild discomfort, while someone with minor changes suffers greatly.
Understanding Degenerative Disc Disease
DDD refers to wear and tear of the discs between your vertebrae (backbones). Over time, discs may thin visibly on imaging. It’s also known as disc osteoarthritis or spondylosis. Think of it as the ‘wrinkling’ of your spine – a natural part of ageing.
Why Discs Degenerate
- Everyone is Affected: It happens universally, but the timeline varies.
- Genetics Play a Role: Some inherit a tendency for earlier DDD onset.
- Ageing Process: Disc changes begin subtly even in childhood, progressing naturally as we get older
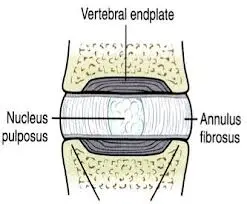
Picture Of A Healthy Disc: Degenerative Disc Disease
Understanding Your Discs: From Healthy to Degenerative
Your spinal discs are more complex than you might think. Let’s break down their structure:
- The Nucleus: The Jelly Center Imagine your disc’s middle is a jelly-like substance called the nucleus.
- The Annulus: The Layered ‘Onion’ The annulus surrounds the nucleus with multiple rings of strong tissue, like the layers of an onion.
- The Endplates: Your Disc’s ‘Mesh’ Floor & Ceiling Picture fine wire mesh covering the bottom and top of your disc – those are the endplates.
How Your Discs Get Nourished
- Childhood: Direct Blood Supply As children, tiny blood vessels tunnel through the endplate mesh, feeding the disc directly with nutrients.
- The Aging Process Sadly, the picture changes in two key ways:
- By age 7: Those blood vessels stop reaching the endplate.[3-5]
- By age 20: The blood vessels through the endplate disappear completely.
Implications of Disc Aging
Without a direct blood supply, nutrients must reach the nucleus by ‘diffusing’ through the jelly and onion layers. This is much slower and less efficient. The effects of this over time are what we call degenerative disc disease. Visible signs on X-rays often start showing up by age 40.
Understanding Disc Degeneration
Internal Pressure and Aging
Your disc bears significant internal pressure to support your body’s weight. Imagine the annulus and nucleus as a balloon filled with water under substantial pressure. However, as you age, a decrease in blood flow, nutrients, and oxygen leads to cell death within the disc.
Decline in Water Content
With fewer cells producing water-retaining molecules, the disc’s water content decreases over time. This reduction in water content results in a decrease in pressure within the disc.
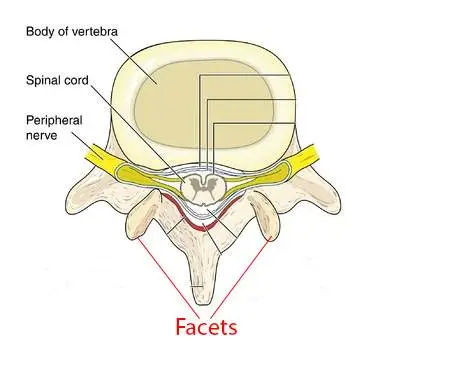
Pressure Redistribution
As the disc “deflates,” pressure shifts from the centre to the back, including the annulus and facet joints. This redistribution of pressure can lead to fissures in the annulus and the development of osteoarthritis in the facet joints.
Disc Herniation
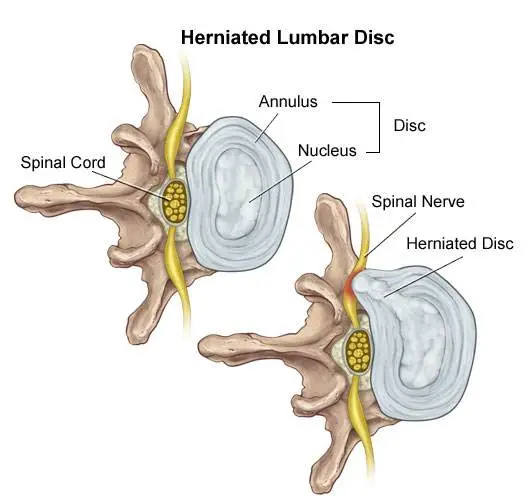
Stage #1 Disc Bulge
- After a few years to a few decades of pressure shifted toward the back of the disc a fissure breaks the many layers of the annulus so that only a few layers of the annulus are left to hold the disc back.
- This allows the nucleus (jelly) to push through the annulus (onion) closer to the edge of the annulus. This is a Disc Bulge ie. the nucleus has been pushed out toward the edge of the annulus.
See Also: Best Treatments To Help Your Lumbar Disc Herniation
Stage #2 Disc Prolapse
- A disc protrusion is like a disc bulge that comes out even more in one focused spot. The disc pushes out as if you had your finger inside a balloon and pushed out.
- A disc protrusion is when the nucleus has pushed through so many layers of the annulus that only one or two layers of the annulus (onion) and a PLL ligament are holding back the nucleus.
- Good news: Severely degenerated discs do not prolapse as there isn’t enough pressure within the disc itself for this to happen.
Stage #3 Disc Extrusion
- A disc extrusion is when the nucleus breaks through the final layers of the annulus and the PLL ligament and pinches on the nerve (spinal nerve).
- In most cases your lower back pain is painful but your sciatica is much worse than your lower back pain.
See Also: Best Exercises For Your Herniated Disc
Vertical Disc Herniation (Smorl’s Node)
- Compression of the spine like lifting very heavy weights, and falling onto your buttock will cause Vertical Disc Herniations in the young.
- When you are young (20 years or under) the annulus is still intact so the weak point becomes the end plate (wire mesh). When you fall and compress your spine severely the annulus is strong enough to withstand tremendous pressure but your weak link is the end plate. The pressure breaks the end plate pushing the nucleus (jelly) into the vertebra below.
- When the nucleus herniates (pushes into) into the vertebra there is more space for the nucleus (jelly) so it’s like deflating a balloon.
- The decreased disc pressure from the disc causes a shift of pressure toward the back of the annulus and the joints (facets) just like a normal disc herniation.
- A Schmorl’s node can be seen on X-ray when the nucleus which has herniated (pushed) into the disc and later on calcifies.
See Also: Your Guide To Disc Bulges, Slipped Discs, Disc Herniations, Disc Protrusion, Disc Extrusions
Why Is My DDD Painful?
Limited Pain Fibers in the Disc
Your disc contains a few pain fibres, primarily located on the outer 1-3 mm of the annulus (the “onion” layer). These fibres typically remain inactive unless the disc is injured.[5]
Onset of Pain
Initially, disc degeneration may occur without causing pain. However, as fissures develop in the outer annulus where the nerve fibres are situated, pain may arise.
Progression of Symptoms
As degeneration progresses, the disc may narrow, develop fissures in the annulus, and potentially form a disc bulge, often leading to persistent pain.
Schmorl’s Node and Pain
The collapse of the end plate, known as a Schmorl’s node, can exacerbate pain by pushing the nucleus (the “jelly” centre) into the adjacent vertebrae, where pain fibres are abundant.
Nerve Growth and Increased Pain
In cases of substantial degenerative disc disease, nerve fibres may grow into the annulus and nucleus, amplifying pain sensations.[6]
Persistent Pain in Disc Herniations
Even in disc herniations, nerve growth into the affected area can contribute to ongoing pain.
Limited Healing Potential
Unlike bones, discs lack the capacity for complete healing following injury, such as a fracture.[2]
Imaging: How To See DDD
#1 X-rays
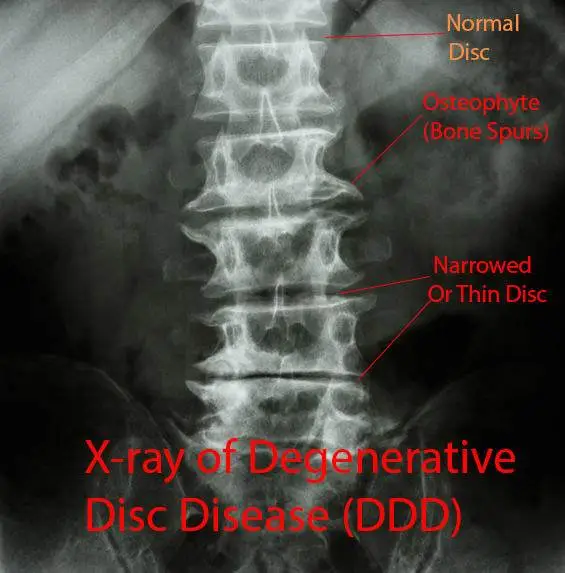
You can see degenerative disc disease on X-rays, CT (CAT) scans and MRI. The most important factors are disc narrowing (smaller), osteophytes (spurs of bone) and disc bulging (seen only on MRI and CT scans)
Often when seen together the radiologist will use the term spondylosis. Most of the time though it may be used to refer to a narrowed disc alone or the presence of multiple osteophytes.
#2 Magnetic Resonance Imaging (MRI)

Magnetic Resonance Imaging (MRI) is the most sensitive tool we have to look at degenerative disc disease. You are looking for disc narrowing, bony spurs called osteophytes, bulging discs and how well the disc is functioning.
MRI Setting T1 and T2
MRI’s have two main settings T1 and T2. The T2 setting shows any tissue that has lots of water in it to show up bright white. The brighter the tissue the more water there is in the tissue.
Normally your disc and spinal cord have a lot of water in so will show up bright white, especially in the nucleus (jelly). As your disc ages, the disc starts to lose water and eventually starts breaking down.
When your disc has substantial degenerative disc disease your disc will no longer look white on a T2 MRI. It will look black since the water has been completely sucked out of the disc. This is called the desiccation of your disc.
#3 Discography

Discography involves injections to try and give you pain in the disc that you think is causing you pain. It’s for people who haven’t responded to non-surgical care and is usually used for planning lumbar fusion surgery.
If your doctor tells you that you need to have a discography you should have serious concerns. First, if you don’t get the surgery it may accelerate disc degeneration and 25% of people are found to have a disc problem when they don’t.[9-10] That’s a huge rate of mistakes.
Remember they are using discography to decide whether they are going to do surgery.
Prevention of DDD
Your mom and dad are the main cause. In other words genetics. Smoking and manual labour are not as important factors for Degenerative Disc Disease. Your parents played the most meaningful part.
The genes that you inherit influence the size, shape and make-up of the vertebrae and disc but also how resilient your disc is.
Degenerative Disc Disease and Disc Herniations
Studies show that if there is a family history of DDD in patients who are diagnosed with a herniated disc before age 21. (Remember you end up with disc herniations as a part of the DDD process)
Frequent Bending, Twisting, Whole Body Vibrations, Smoking and Blood Flow affect
The minor factors which put you at risk for degenerative disc disease are frequent bending and twisting, whole body vibration, [11] smoking from nicotine and impaired blood flow to the disc [12-15] and association of plaques in the arteries called atherosclerosis in the main artery in the lower back [16]
Heavy lifting is associated with disc prolapse but not other areas of degenerative disc disease
Treatment For Degenerative Disc Disease
The golden rule is to always try non-surgical care first. Spinal manipulation by a chiropractor, McKenzie Method approach and lower back stabilization exercises have been shown to relieve pain.[17-18]
Traction and spinal decompression is ineffective for treating degenerative disc disease.
Surgical Options for Degenerative Disc Disease
1. Fusion Surgery (Arthrodesis)
Spinal fusion surgery entails the removal of the nucleus and a significant portion of the annulus. Bone grafts from the pelvis are transplanted to fuse the adjacent vertebrae, creating a single unit.
- Effectiveness and Risks: While fusion surgery can alleviate pain in some cases, it often accelerates degeneration in nearby vertebrae, particularly within a decade post-surgery.[19-21]
- Patient Awareness: Surgeons should provide comprehensive information on the pros and cons of fusion surgery to patients. Failure to do so may raise concerns.
- Concerns about Bone Morphogenetic Protein (BMP): BMP, used as a bone graft substitute, has been associated with potentially life-threatening complications, as highlighted by an FDA public health notification in 2008 [25].
- Comparative Studies: Despite being a standard practice in Europe, studies indicate that fusion surgery may not offer significant advantages over exercise therapy and cognitive therapy in both short and long-term outcomes [26].
2. Total Disc Replacement for Degenerative Disc Disease
Total Disc Replacement involves replacing the problematic disc with an artificial one. However, concerns exist regarding the long-term durability of polyethene [22-23] components and the prevention of adjacent vertebrae wear and tear.
- Motion and Adjacent Vertebrae: Some studies suggest a complete loss of motion at the operated level due to fusion between the artificial segment and the bones[27]. Additionally, evidence does not support the notion that artificial discs reduce degeneration in adjacent vertebrae.
- Risks: Complications such as blood clots or bleeding from injured blood vessels can lead to fatalities following total disc replacement surgery.
Feel free to share your questions, thoughts and experiences in the comments below, and don’t forget to connect with us on Facebook for more updates and tips on improving your health. We’d love to hear your opinions on who you consider the best Toronto chiropractor.
References
1. Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. Journal of Bone and Joint Surgery—Series A. 1990;72(8):1178–1184.
2. Adams MA & Roughley PJ, What is intervertebral disc degeneration, and what causes it?, Spine 2006; 31(18): 2151-2161.
3. Taylor JR , Growth of human intervertebral discs and vertebral bodies. J Anat. 1975 Sep; 120(Pt 1):49-68.
4. Holm S, Maroudas A, Urban JPG, et al. Nutrition of the intervertebral disc. Solute transport and metabolism. Connect Tiss Res. 1981;8:101–119. doi: 10.3109/03008208109152130.
5. Maximilian Rudert and Bemhard Tillmann, Lymph and blood supply of the human intervertebral disc Cadaver study of correlations to discitis Acta Ofthop Sand 1993; 64 (1): 37-40
References
6. García-Cosamalón J, del Valle ME, Calavia MG, et al. Intervertebral disc, sensory nerves and neurotrophins: who is who in discogenic pain? Journal of Anatomy. 2010;217(1):1–15.
7. Sowa G, Vadalà G, Studer R, et al. Characterization of intervertebral disc aging: longitudinal analysis of a rabbit model by magnetic resonance imaging, histology, and gene expression. Spine.2008;33(17):1821–1828.
8. Prescher A. Anatomy and pathology of the aging spine.European Journal of Radiology. 1998;27(3):181–195.
9. Carragee EJ, Tanner CM, Khurana S, et al. The rates of false-positive lumbar discography in select patients without low back symptoms. Spine. 2000;25(11):1373–1381.
10. Carragee EJ, Don AS, Hurwitz EL, Cuellar JM, Carrino J, Herzog R. 2009 ISSLS prize winner: does discography cause accelerated progression of degeneration changes in the lumbar disc: a ten-year matched cohort study. Spine. 2009;34(21):2338–2345.
References
11. Lötters F, Burdorf A, Kuiper J, Miedema H. Model for the work-relatedness of low-back pain. Scandinavian Journal of Work, Environment and Health. 2003;29(6):431–440.
12. Battié MC, Videman T. Lumbar disc degeneration: epidemiology and genetics. Journal of Bone and Joint Surgery—Series A. 2006;88(supplement 2):3–9.
13. Battie MC, Videman T, Gill K, et al. 1991 Volvo Award in Clinical Sciences: smoking and lumbar intervertebral disc degeneration: an MRI study of identical twins. Spine.1991;16(9):1015–1021.
14. Oda H, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y, Iwahashi M. Degeneration of intervertebral discs due to smoking: experimental assessment in a rat-smoking model. Journal of Orthopaedic Science. 2004;9(2):135–141.
15. Iwahashi M, Matsuzaki H, Tokuhashi Y, Wakabayashi K, Uematsu Y. Mechanism of intervertebral disc degeneration caused by nicotine in rabbits to explicate intervertebral disc disorders caused by smoking. Spine. 2002;27(13):1396–1401.
References
16. Kurunlahti M, Tervonen O, Vanharanta H, Ilkko E, Suramo I. Association of atherosclerosis with low back pain and the degree of disc degeneration. Spine. 1999;24(20):2080–2084.
17. Adams MA & Roughley PJ Spine 2006; 31(18): 2151-2161. What is intervertebral disc degeneration, and what causes it?
18. Beattie P upon etiology, pathophysiology, and lumbar Magnetic Resonance Imaging Journal of Orthopaedic & Sports Physical Therapy 2008; 38(6): 329-340.
19. Song K-J, Choi B-W, Jeon T-S, Lee K-B, Chang H. Adjacent segment degenerative disease: is it due to disease progression or a fusion-associated phenomenon? Comparison between segments adjacent to the fused and non-fused segments. European Spine Journal. 2011;20(11):1940–1945. [PMC free article] [PubMed]
20. Tang S, Rebholz BJ. Does anterior lumbar interbody fusion promote adjacent degeneration in degenerative disc disease? A finite element study. Journal of Orthopaedic Science.2011;16(2):221–228. [PubMed]
References
21. Wu JC, Liu L, Wen-Cheng H, et al. The incidence of adjacent segment disease requiring surgery after anterior cervicaldiskectomy and fusion: estimation using an 11-year comprehensive nationwidedatabase in Taiwan. Neurosurgery. 2012;70(3):594–601.
22. Delamarter R, Zigler JE, Balderston RA, Cammisa FP, Goldstein JA, Spivak JM. Prospective, randomized, multicenter food and drug administration investigational device exemption study of the ProDisc-L total disc replacement compared with circumferential arthrodesis for the treatment of two-level lumbar degenerative disc disease: results at twenty-four months. Journal of Bone and Joint Surgery—Series A. 2011;93(8):705–715.
23. Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine. 2008;33(15):1701–1707.
24. Center for Devices and Radiological Health. FDA public health notification: life-threatening complications associated with recombinant human bone morphogenetic protein in cervical spine fusion, 2011.
25 Ritzell P, Hagg O, Wessberg P, Nordwall A. Swedish Lumbar Spine Study Group. Lumbar fusion versus non-surgical treatment for chronic low back pain: a multicentre randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine. 2001;26:2521–32.
26. Guyer RD, McAfee PC, Hochschuler SH, Blumenthal SL, Fedder IL, Ohnmeiss DD, Cunningham BW Prospective randomized study of the Charite artificial disc: data from two investigational centers, Spine J. 2004 Nov-Dec; 4(6 Suppl):252S-259S.